So You Want to Recommend Yoga to your Client with Depression
“So You Want to Recommend Yoga to your Client with Depression,” by Marie Chesaniuk, PhD
By now, yoga has become ubiquitous in American culture. Over 33 million Americans are estimated to have participated in yoga in 2023. The conversation about yoga has long referenced its relaxing nature, low key physical activity, and positive influence on general wellbeing. There is also growing research data suggesting yoga can be a beneficial complementary or integrative therapy for depression. So, knowing all this, you want to recommend yoga to your client with depression.
But like…how much yoga are we talking here? How often? Does it matter what type of yoga? Does it matter what type of depression? Do you mean a class or independently at home? How much should I expect it to decrease depression symptoms? Which ones? Does it only help general wellbeing, but nothing depression-specific? How? What is it about yoga that helps in the treatment of depression? What is the perfect treatment combination for depression? Is it psychotherapy plus yoga? Psychotherapy, medication, plus yoga? Can yoga replace psychotherapy and/or medication? Is yoga ever not beneficial? For who?
Do you need to take some deep breaths in child’s pose now? Worry not! I read a pile of meta-analyses, so breathe in through your nose, reach out with your hands, and settle deeper into the details on yoga for depression.
What kind of yoga?
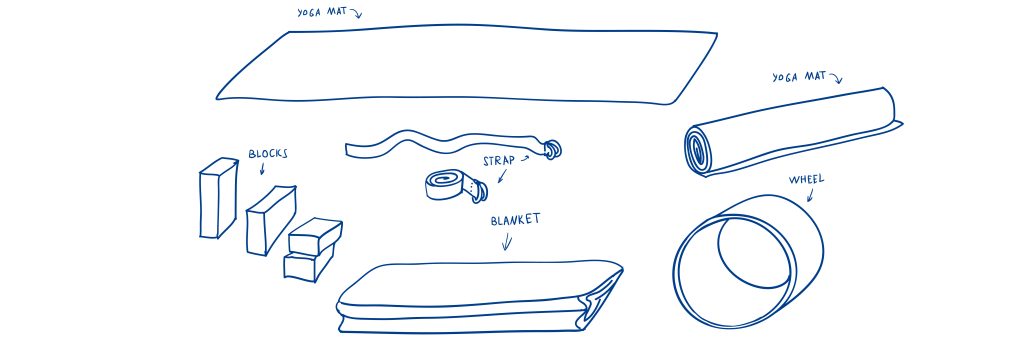
Most yoga used in interventions involved poses and the movements to get into, hold, and transition out of them (asana), breathwork (pranayama), and/or mindfulness (e.g., meditation, relaxation.) The most common style of yoga referenced was Hatha yoga, followed by a smattering of studies that included Iyengar yoga, laughter yoga, Yoga Nidra, Sudarshan Kriya yoga, Ashtanga yoga or simply referenced “yoga” without describing their approach. Yoga approaches that included meditation or relaxation in addition to physical exercises showed some benefit over yoga approaches not incorporating these elements. However, there is insufficient research on yoga approach and depression to make a recommendation beyond seeking an approach that integrates asana, pranayama, and mindfulness.
How much yoga? How often?
The base recommendation is 60 minutes of yoga per week for 8 weeks, but there has been some evidence of a dose-response relationship in which greater reductions in depressive symptoms were associated with more yoga sessions per week. Due to limited research, it is unknown whether there is a point of diminishing returns where the benefit of yoga would plateau and/or reverse.
Some studies found a shorter-term yoga intervention (<8 weeks) was more beneficial to people with depression than longer term (>8 weeks) intervention, but the data is sparse. The takeaway here is that a person with depression could benefit from a couple months of weekly hour-long integrated yoga classes (the vast majority of studies used group-based yoga interventions) without committing to a long term yoga lifestyle change.
What kind of depression?
The evidence is mixed when it comes to level of severity. Some studies found no or less benefit among people with more severe depression. Some studies found that those with subclinical depression symptoms most commonly reported greater reduction in depressive symptoms than those with a formal diagnosis or more severe depression, but not in every study. This detail remains unclear due to differences in recruiting those who have or have not received a formal diagnosis. Maybe recruiting people with formally diagnosed depression captures a group of people who are different in important ways from those recruited from the community without a formal diagnosis. The available research is missing information on this issue and it remains inconclusive. If you recommend yoga to your client with depression, you may want to set realistic expectations of how much benefit (if any) they should expect from yoga. Based on the data available, they stand a good chance of reducing symptoms of depression by incorporating yoga into their mental health treatment regimen, but there are no guarantees and results may vary from person to person.
How does yoga impact symptoms of depression? What is the mechanism of change?
There is increasing information about what happens between practicing yoga and decreasing depressive symptoms. Thus far, studies have shown that yoga positively impacts neurotransmitters involved in depression (e.g., increased gamma-aminobutyric acid (GABA) levels, increased dopamine release, and increased plasma serotonin.) It can decrease physiological stress responses (e.g., improved regulation of the hypothalamic-pituitary-adrenal (HPA) axis, decrease in plasma cortisol, promotion of frontal electroencephalogram (EEG) alpha wave activity, which facilitates relaxation, and increased vagal tone.) These changes may lead to the end result of decreased depressive symptoms, although there is much to be learned and replicated still.
How does yoga compare to therapy?
One meta-analysis found that effects of yoga on mental health were similar to that of pharmacological treatment, group therapy, social support groups, and massage. Another meta-analysis found that yoga as an adjunct combination with medication was more effective in improving severe depression alone. Both of these findings have some major caveats. We know far more about the effects of common antidepressant medications (e.g., SSRIs) and psychotherapy (e.g., cognitive behavioral therapy) in much finer detail and across both short and long terms than we do about the effect of yoga on depression or even mental health more generally. It seems that yoga presents a promising (or at least low risk, given the absence of adverse event reports in studies) adjunct to better-supported treatments for depression, not a replacement for them.
Who does not benefit from yoga?
No meta-analysis reviewed reported an increase of depression symptoms in any study group. However, some reported groups of participants who either had no benefit or less of a benefit than others. Participants located in India showed less of a benefit compared to those located in the USA, suggesting cultural differences. There was mixed evidence regarding whether people benefit more or less depending on severity of depression symptoms. Missing data on participant characteristics including attitudes about yoga, prior and/or simultaneous yoga practice and treatment of depression, and outcome expectancies among other information would move us toward finding the limitations of yoga for depression.
Limits of Available Evidence
Beyond the missing participant and yoga intervention characteristics mentioned above, there are numerous other challenges to getting good information on this topic. High quality studies have been hampered by the difficulty in blinding participants and study staff to the yoga and comparison groups. The ubiquity of yoga makes it pretty tough to hide from study participants and staff! While evidence is building, comparisons to multiple control and alternate treatment groups is still lacking as is replication. This makes it impossible to draw strong conclusions and make strong, tailored recommendations to clients.
What’s the Recommendation?
Sixty minutes per week of group yoga with elements of asana, pranayama, and mindfulness for at least 8 weeks may decrease depressive symptoms in conjunction with other evidence-based treatment for depression, like medication and psychotherapy. The risk for harm is low given the absence of adverse event reports. Consider taking pre- and post-yoga intervention measures of depression symptoms using a validated inventory to help you and your client fill in the blanks in the ongoing research base and better characterize whether and how your client with depression benefits from yoga.
Sources:
Brinsley, J., Schuch, F., Lederman, O., Girard, D., Smout, M., Immink, M. A., ... & Rosenbaum, S. (2021). Effects of yoga on depressive symptoms in people with mental disorders: a systematic review and meta-analysis. British journal of sports medicine, 55(17), 992-1000.
Cramer, H., Lauche, R., Langhorst, J., & Dobos, G. (2013). Yoga for depression: A systematic review and meta‐analysis. Depression and anxiety, 30(11), 1068-1083.
Gong, H., Ni, C., Shen, X., Wu, T., & Jiang, C. (2015). Yoga for prenatal depression: a systematic review and meta-analysis. BMC psychiatry, 15, 1-8.
Klatte, R., Pabst, S., Beelmann, A., & Rosendahl, J. (2016). The efficacy of body-oriented yoga in mental disorders: A systematic review and meta-analysis. Deutsches Ärzteblatt International, 113(12), 195.
Rhoads, M. C., Grevstad, N., Kirkland, R. A., Barber, M. E., Myers, S., & Lundstrom, T. (2023). The benefits of yoga as an intervention for depression: a meta–analysis. Int J Complement Alt Med, 16(1), 19-30.
Vollbehr, N. K., Bartels-Velthuis, A. A., Nauta, M. H., Castelein, S., Steenhuis, L. A., Hoenders, H. R., & Ostafin, B. D. (2018). Hatha yoga for acute, chronic and/or treatment-resistant mood and anxiety disorders: A systematic review and meta-analysis. PLoS One, 13(10), e0204925.
Wu, Y., Yan, D., & Yang, J. (2023). Effectiveness of yoga for major depressive disorder: A systematic review and meta-analysis. Frontiers in psychiatry, 14, 1138205.
About Us
Learn moreOur Care
Learn moreWhat We Treat
Learn more